Health is an intrinsic value and a precondition for pursuing a good quality of life. Whilst universal healthcare provides equitable health to the population, most healthcare systems have strategies to improve healthcare services while reducing costs. [1][2] Value-Based Healthcare (VBHC), or care delivered under value-based contracts, provides promise due to its potential for better care. [3] VBHC prioritises collaboration, among healthcare professionals to provide tailored care that addresses their individual requirements. This approach acknowledges healthcare as a multifaceted system and understands the specific needs of patients’ while considering the costs needed to achieve this. [3]
Under a VBHC model, healthcare services provided by hospitals, laboratories, doctors, nurses, and others are reimbursed based on the health-outcomes of their patients and the quality of services rendered. [3] Though no agreed upon definition, the goal of VBHC and generating value evidence is to maximise the ‘value of care for patients’ and reduce the overall cost of healthcare. [4] Research over the years have focused on both the results and costs aspects of Porter’s value equation. The equation [Figure 1] proposes that healthcare should aim for ‘value’, which is determined by dividing desirable and relevant patient outcomes by the cost of providing care. [5]
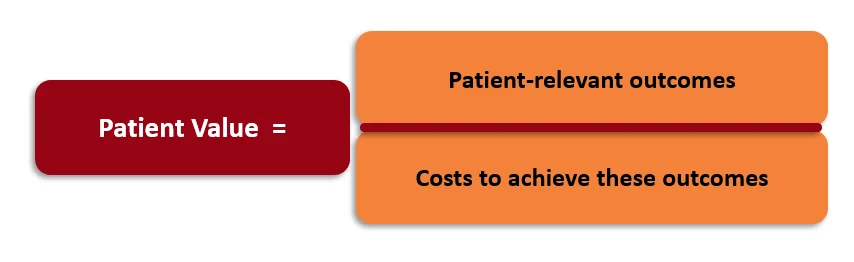
Figure 1. Value-Based Healthcare (Porter 2020)
Comparing Old Reimbursement Models
Historically, healthcare reimbursement follows a Fee for Service (FFS) model, which is a system of healthcare payment where provider payments are separate for each service rendered. It drives volume and not value, as payments depend on quantity, not quality. [6][7] The FFS model is one of the major drivers of the high costs of healthcare. It promotes the use of more tests, procedures and treatments and contributes to the decline in primary-care workforce. [8]
The transition to VBHC based on patient outcomes (i.e., valued based care vs fee-for-service), is a strategy that encourages quality rather than quantity. It shifts the focus on care of individuals to services that keep societies healthy, reducing overall costs on healthcare. [6] Healthcare providers (HCPs) receive financial rewards for positive patient outcomes, efficient delivery of care, and are encouraged to engage with patients, giving them a connected care experience. VBHC also promotes a coordinated team approach to improve efficiency and patient satisfaction. [9]
New Models Based on VBHC
Although many efforts have been made to improve the value in healthcare systems, historically they have failed to improve results and control costs. Porter and Teisberg suggested an extensive redesign of the healthcare system called the “value agenda”, with an emphasis on competition and enhancement. They suggested a singular overarching objective for healthcare: providing value to the patient. This six-component system includes five actions underpinned by a supporting information technology platform [Figure 2]. It leads to value in healthcare by obtaining the best clinical outcomes and patient experience, at the lowest cost. [10] [11]

Figure 2. The Value Agenda (Porter, 2020)
Why is Value-Based Healthcare Important?
VBHC offers a radical transformation of healthcare systems. It enables transitioning from volume-based to value-based healthcare delivery and payment systems. This approach focuses on the ‘quality of care’ and the overall wellness of the patient, with better outcomes as key for compensation. [12]
The following highlights the significance of VBHC [6][9]:
- Efficiency and prevention: Healthcare services are focused on attempting to cure patients and not merely managing disease as well as implementing preventative strategies to avoid preventable diseases.
- Integrates service delivery: HCPs combine collective resources and expertise with a critical analysis into a single platform, creating a holistic picture of a patient’s care; collaborative healthcare leads to efficiency improvements. Implementation of a collaborative approach also contributes to reduced medical errors.
- Improves Societal Health: By reducing healthcare expenditures and prioritising preventative medicine and better management of chronic conditions, funds can be reallocated to other sectors of society, resulting in increased patient satisfaction and improved societal health.
- Reduces payer costs: With an emphasis on prevention and fewer HCP visits, payer costs will reduce, lessening the effects on premium pools and investments. The reduction in exposure and risk increases the financial health of the payer.
Collaboration in Value-based Healthcare
At the centre of a VBHC system, is a robust multidisciplinary team which comprises of pharmacists, dieticians, case managers, mental health specialists, administrators, and others. They work together with the patient and caregiver to identify and address the individual healthcare needs of each patient. [3] Collaboration in VBHC involves connecting two or more stakeholders to enhance the value delivered to the system and society by enhancing patient outcomes in a manner that is mutually advantageous and decreases the system’s burden. This involves moving away from the “every person for themselves” mindset and recognising that cooperation may lead to mutual benefits for everybody. [13]
To implement VBHC, multidisciplinary teams (MDT) must contribute their knowledge and practical experience, which stimulates the creation of innovation. This level of involvement can yield significant advantages by reducing hospital demands and enhancing patient outcomes. Cancer management is a prime illustration of how these various VBHC models can have a beneficial effect. Effective cancer care involves close communication among trained oncologists, secondary and tertiary care providers, and laboratories collaborating to determine the best treatment for patients. Shifting cancer treatment to community settings decreases hospital involvement and improves accessibility. Comparable advantages have been shown in chronic disease management including in obesity and atrial fibrillation using MDTs. [13]
Value-Based Health Care Implementation Framework
A strategic framework seen in [Figure 3] may assist organisations with building VBHC systems. This framework involves understanding the shared health needs of patients and organising service provision around these needs. Therefore, it is different from the current models, where services are organised around service providers. The framework suggests that health care should be structured around patient segments with similar health needs, such as “people with knee pain” or “elderly people with multiple chronic conditions.” It also emphasises the importance of designing comprehensive solutions for patients’ needs, integrating learning teams, measuring health outcomes and costs, and expanding partnerships. Comprehensive solutions may address both clinical and nonclinical needs of patients, while integrated learning teams can ensure effective and efficient care. This framework can lead to better health outcomes, usually at lower overall costs, and provide opportunities for expanded partnerships, ultimately serving more patients. [14]
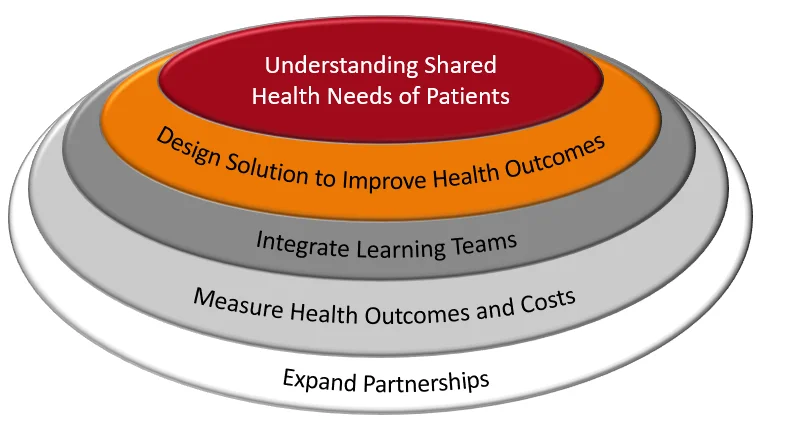
Figure 3. Strategic Framework for Value-based healthcare implementation (Teisberg et al. 2020)
Who benefits from VBHC?
Multiple stakeholders involved in the health care system—from patients and clinicians to health plans and employers—share a common goal: reducing healthcare costs without sacrificing quality of treatment. For example, employers are more willing to engage in direct contracts with HCPs and pay higher fees for care that is evidenced to have fewer complications and enables employees to return to work sooner. This is because quicker and more complete recovery helps reduce other costs for the employer, such as those related to employee absenteeism. By structuring treatment around VBHC, it also increases efficiency by eliminating the need for physicians to attend to routine tasks such as constantly coordinating basic services. The increased bandwidth and optimisation of physician services, enables more specialised care including personalised healthcare. Better outcomes associated with VBHC cuts costs for the payers as it minimises illness complexity and need for more care. A diabetic, as examples, who does not develop renal failure or diabetic polyneuropathy, saves significant costs over time. [14]
Where does the Patient Fit?
VBHC is a patient-centric model at its core with the aim to improve outcomes while also reducing costs. [13] It is organised around patients with shared needs while demonstrating better value in care creates opportunities and improves health outcomes for more people. [14] A patient-centric model [Figure 4] that aligns the patient’s needs with the interests of healthcare provider, focuses on an integrated approach to patient care. [15] Healthcare facilities need to transform into patient-centred systems that integrate patient input into the decision-making processes to enhance care and health results. Integrated practice units (IPUs) focus on a multidisciplinary, comprehensive, holistic plan that addresses the complete cycle of care, mostly utilised in cancer care.
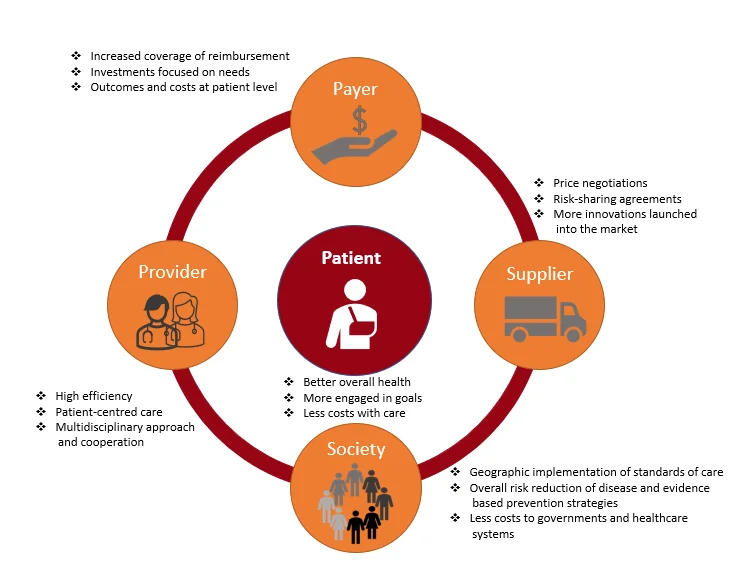
Figure 4. Benefits to the patient of value-based healthcare (Redondo et al. 2019)
Benefits of Value-Based Healthcare
VBHC offers advantages to patients, providers, payers, suppliers, and society as a whole [Figure 5] [6][9]:
- Patients spend less money to achieve better outcomes.
VBHC focuses on the management of chronic diseases as well as assisting patients recover from illness or injuries more rapidly. This results in fewer tests, doctor visits, and prescriptions, with improved outcomes at a lower cost. - Providers achieve efficiency and greater patient satisfaction.
Quality of care and patient engagement increases when HCPs are focusing on value instead of volume. In addition, it rewards providers for their efforts to generate higher value per episode of care. - Payers reduce risk and control cost.
A healthier population with fewer healthcare claims reduces premium pool and investment strain. Value-based payment allows payers to boost efficiency by bundling payments for the patient’s whole treatment cycle or chronic diseases over a year. - Suppliers align prices with patient outcomes.
Suppliers and manufacturers align their products and services with positive patient outcomes. Many healthcare stakeholders want manufacturers to price pharmaceuticals based on their patient value, which will be streamlined with personalised therapies. - Healthier societies with reduced overall healthcare spend.
Societies with lower costs of managing chronic diseases also have lower costly hospitalisations and medical emergencies and, as a result, less overall spend on healthcare.

Figure 5. Value-Based Healthcare Benefits by Stakeholder (NEJM Catalyst, 2017)
Enables and Barriers of Value-based Healthcare
VBHC is still evolving, and ways of improving the model are ongoing. Key enablers include strong government involvement in healthcare, continuous improvement of information technology (IT) infrastructure, and the implementation of a value-based culture among providers. Government support, seed funding, and rewards for high-value care are crucial. An effective IT system should support information flow across care pathways. Providers, particularly physicians, need to understand and support the transition to new models for successful implementation. However, barriers exist, such as the increased financial risk for providers who are reimbursed based on health outcomes, not per-visit payments. Moreover, healthcare’s highly regulated nature can cause issues such as measuring health outcomes, ensuring patient data safety, establishing new payment models, and holding pharmaceutical, biotech companies, and infrastructure providers accountable. [16][17]
Conclusion
In conclusion, VBHC represents a transformative approach to healthcare delivery that prioritises patient outcomes and cost-effectiveness. It offers significant benefits to patients, providers, payers, suppliers, and society as a whole by focusing on prevention, efficient service delivery, and improved societal health. The implementation of VBHC necessitates a collaborative, multidisciplinary approach that caters to the specific needs of patients. Despite the challenges associated with its implementation, such as increased financial risk for providers and regulatory issues, VBHC has the potential to enhance healthcare systems globally. As VBHC continues to evolve, ongoing research and policy development will be crucial to address these challenges and maximise the benefits of this innovative model.
References
- Zipfel N, van der Nat PB, Rensing BJWM, Daeter EJ, Westert GP, Groenewoud AS. The implementation of change model adds value to value-based healthcare: a qualitative study. BMC Health Serv Res. 2019 Sep 6;19(1):643. doi: 10.1186/s12913-019-4498-y.
- European Commission, Directorate-General for Health and Food Safety, Defining value in ‘value-based healthcare’ – Opinion by the Expert Panel on effective ways of investing in Health (EXPH), Publications Office, 2019, Available: https://data.europa.eu/doi/10.2875/148325 [Accessed 24 Feb 2024]
- AETNA, “Better health at lower costs: Why we need Value-Based Care now,” 2021. [Online]. Available: https://www.aetna.com/employers-organizations/resources/value-based-care.html [Accessed 24 Feb 2024].
- What is Value Based Healthcare? Read about Michael Porters definition [Internet]. Consultancy in Healthcare and Life Sciences | Vintura Consultancy. Available from: https://www.vintura.com/value-based-healthcare/michael-porter/ [Accessed 22 Feb 2024].
- Porter, M.E. Value-Based Health Care Delivery: Core Concepts. Presented Partners HealthCare Residents and Fellows Course. 15 January 2020. Boston, MA. (2020). [Accessed 21 Feb 2024]. Available from: https://cdn.ymaws.com/www.amwa.org/resource/resmgr/journal/Issues/2013/2013v28n3_online.pdf
- Value Based Healthcare and Why It’s Important:What Agents Should Know and Share with Clients [Internet]. [Accessed 26 Feb 2024]. Available from: https://redbirdagents.com/value-based-healthcare-and-why-its-important/
- What is Value-Based Care? [Internet]. [Accessed 26 Feb 2024]. Available from: https://www.huffpost.com/entry/what-is-value-based-care_b_58939f9de4b02bbb1816b892
- INSIGHT: The Healthcare Industry’s Shift from Fee-for-Service to Value-Based Reimbursement [Internet]. [Accessed 26 Feb 2024]. Available from: https://news.bloomberglaw.com/health-law-and-business/insight-the-healthcare-industrys-shift-from-fee-for-service-to-value-based-reimbursement
- NEJM Catalyst. What Is Value-Based Healthcare? Catal Carryover [Internet]. 2017 Jan [Accessed 26 Feb 2024]. Available from: https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0558
- Key Concepts – Institute For Strategy And Competitiveness – Harvard Business School [Internet]. [Accessed 26 Feb 2024]. Available from: https://www.isc.hbs.edu/health-care/value-based-health-care/key-concepts/Pages/default.aspx
- Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Boston: Harvard Business School Press; 2006.
- Putera I. Redefining Health: Implication for Value-Based Healthcare Reform. Cureus. 2017 Mar 2;9(3):e1067. doi: 10.7759/cureus.
- Collaborating for better outcomes [Internet]. Eradigm Consulting. 2022 [Accessed 22 Feb 2024]. Available from: https://eradigm.com/white-paper/collaborating-for-better-outcomes/
- Teisberg E, Wallace S, O’Hara S. Defining and Implementing Value-Based Health Care: A Strategic Framework. Acad Med. 2020 May;95(5):682-685. doi: 10.1097/ACM.0000000000003122.
- Redondo P., Ribeiro M, Lopes M, Borges M, Gonçalves F.R (2019) Holistic view of patients with melanoma of the skin: how can health systems create value and achieve better clinical outcomes? ecancer 13 959
- Mjåset C, Ikram U, Nagra NS, Feeley TW. Value-Based Health Care in Four Different Health Care Systems. Catal Non-Issue Content [Internet]. 2020 Nov 10 [Accessed 26 Feb 24]. Available from: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0530
- DelveInsight. What Is Value-Based Healthcare? | Value-Based Care | VHBC System [Internet]. DelveInsight Business Research. 2020 [Accessed 26 Feb 2024]. Available from: https://www.delveinsight.com/blog/value-based-healthcare
Table of Contents
