Introduction
Over the past half century, cardiovascular diseases (CVDs) have become the leading cause of death and premature deaths globally. From mid-1970, an unexpected decline in mortality due to CVDs, including major vascular diseases such as coronary heart disease (CHD) and stroke, was reported. In high-income countries a global public health favourable trend was achieved in CVDs with mortality levels typically falling by 40-80%. By the year 2000, the age-adjusted CHD mortality rates declined to a third of their 1960 baseline. In the United States of America (USA), the annual age adjusted CVD mortality rates continued to decline by 22% from 1990 to 2013. Other high-income countries, including Western Europe, Japan, New Zealand and Australia have reported similar trends with over 70% decline reported in the Netherlands and over 60% in the United Kingdom (UK) and Ireland.
From studies, we could attribute this trend to several factors, including exposure to risk factors, improved medical management and screening, as well as technology advances [1][2]. The key to cardiovascular disease burden reduction depends on cardiovascular disease innovations and therefore patients should have access to appropriate technology, medication and medical devices to treat CVDs. We briefly describe 7 of the important cardiology discoveries of the 20th century as these are fundamental to the extraordinary strides made in the basic cardiovascular science and development of new diagnostic and therapeutic techniques.
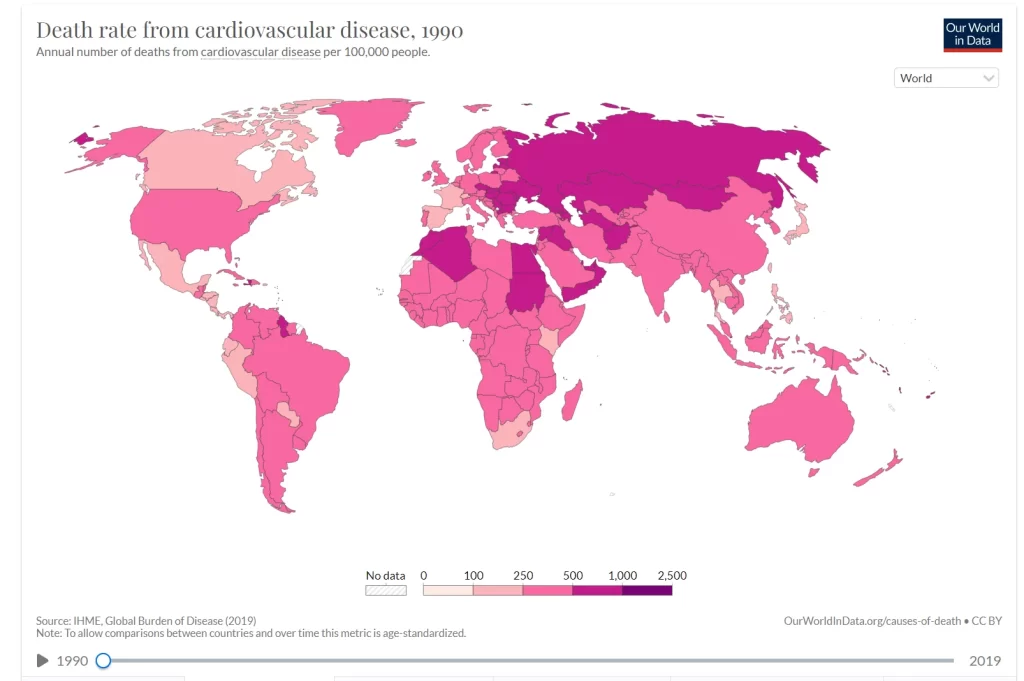
Source: IHME, Global Burden of Disease (2019)
Cardiovascular Disease Innovations
Electrocardiography
“I do not imagine that electrocardiography is likely to find any very extensive use in the hospital. It can be at most of rare and occasional use to afford a record of some rare anomaly of cardiac action” – was the words of Augustus Waller who was the pioneer in electrocardiography in 1911. It was, however, 13 years later that the Nobel Prize in Medicine was awarded to the father of electrocardiography, Willem Einthoven, who was able to transform this technology into an indispensable clinical recording tool still used in our current practices. In 1887, Einthoven attended the International Congress of Physiology in London, where Waller demonstrated the use of a capillary electrometer to record an “electrograph”. From then, Einthoven explored the use of capillary electrometers to record minute electrical currents. After 10 years of research and clinical studies, the potential of electrocardiography was realised. It was used to diagnose arrhythmias, the association of T-wave inversion with angina and arteriosclerosis was identified in 1910. His contributions also formed the foundation for several other important discoveries made during the 20th century.
Echocardiography
During World War II, the use of ultrasonography was advancing rapidly because of its use for detection of submarines. In 1954, Inge Edler and Hellmuth Hertz borrowed a sonar from a local shipyard and adapted it in order to record continued movements of the heart walls. Edler was a cardiologist at Lund University in Sweden and Hertz was a Swedish physicist. They used the improved sonar device to record cardiac echoes from Hertz’s own heart and described the use of ultrasonic cardiogram for mitral valve disease in 1956. Further developments included Doppler echocardiography in 1960, which also included the invention of the ink-jet printer (another invention from Hertz). Edler and Hertz were joint recipients of the Lasker Prize (equivalent to the American Nobel Prize in Medicine) in 1977. In Germany, Sven Effert used cardiac ultrasound to detect left atrial masses from 1959, who later went to the USA to discuss the potential of ultrasonography and its advantages. The first book on echocardiography was written by Harvey Feigenbaum in 1972, who was also the lead of the research team of cardiac ultrasonography in Indianapolis.
Coronary angioplasty
The first balloon angioplasty was performed in 1977 by Greuntzig (a German radiologist and cardiologist) on a 37-year-old man who had consented to angioplasty even after being informed that he would be the first patient to receive this experimental procedure. Initially, the techniques for relieving stenosis in the iliofemoral arteries with dilators were largely ignored in the USA because of technical difficulties and complications. The Greuntzig technique of percutaneous transluminal coronary angioplasty (PTCA) took the cardiology community by storm and was the beginning of the interventional cardiology era. An international registry for PTCA has been established to provide a method for systemic evaluation. In 1997, angioplasty was recognised as a standard procedure in hospitals globally.
Automatic implantable cardiac defibrillators
The first successful attempt at electrical defibrillation was in 1775, when a Danish veterinarian evaluated the effect of electrical shock on chickens. However, the original concept of the artificial pacemaker would be attributed to Albert Hyman, who published a paper on this topic in 1932. It was only 15 years later that the first electrical defibrillation application on the human heart took place and the first commercial pacemaker was designed in 1950. Several early devices were developed and led to the invention of an automatic implantable cardiac defibrillator (AICD). This design was aimed at aborting the ventricular fibrillation at its onset, thus, to avert a fatal outcome. The concept initially generated a lot of criticism, but in 1980, after extensive research on animals, the first human was treated with AICD. With low mortality rates seen, this soon became the treatment of choice for patients with life-threatening ventricular tachyarrhythmias [3].
Beta blockers
Over the years, few drug groups have been studies as widely as beta-blockers in different cardiovascular conditions. In 1950, Sir James Black, a pharmacologist, discovered propranolol and is considered being one of the most important contributions to the clinical and pharmacology field from the 20th century. He received the Nobel Prize in Medicine in 1988 and his conclusions and methods or research have continued to influence cardiovascular medicine [4].
Angiotensin converting enzyme (ACE) -inhibitors
This drug class, often prescribed in cardiovascular disease, was discovered in 1975 by Nobel Prize winner John Vane. The first ACE inhibitor, Captopril, was derived from snake venom after Vane initially tested peptides from venom on dog lungs, finding that they were able to inhibit the activity of angiotensin converting enzyme. Captopril was based on the venom of the poisonous Brazilian Viper (Bothrops Jararaca) but is rarely still prescribed in modern medicine due to the subsequent development of other drugs in this class.
Statins
In 1978, Alfred Alberts, a biochemist, discovered lovastatin in oyster mushrooms, which forms the basis for the development of statin therapy today. The history, however, can be dated back to 1970, where a Japanese microbiologist Akira Endo isolated the first known compound to lower cholesterol from Penicillium citrinum. This compound, called mevastatin was tested to successfully lower cholesterol in animals but was considered to be toxic for human use [5].
Global Initiatives
Despite all the advances made in the field of cardiology, CVDs are still the leading cause of death according to the World Health Organisation (WHO) with an estimated 17.9 million people per year affected. This represents 32% of all global deaths and over three quarters of the deaths occur in low- and middle-income countries. Most CVDs can be prevented and treated by addressing behavioural risk factors and access to early detection as well as management with counselling and medicine. Evidence is emerging that CVDs contribute to poverty because of catastrophic health spending and a high out-of-pocket burden for healthcare.
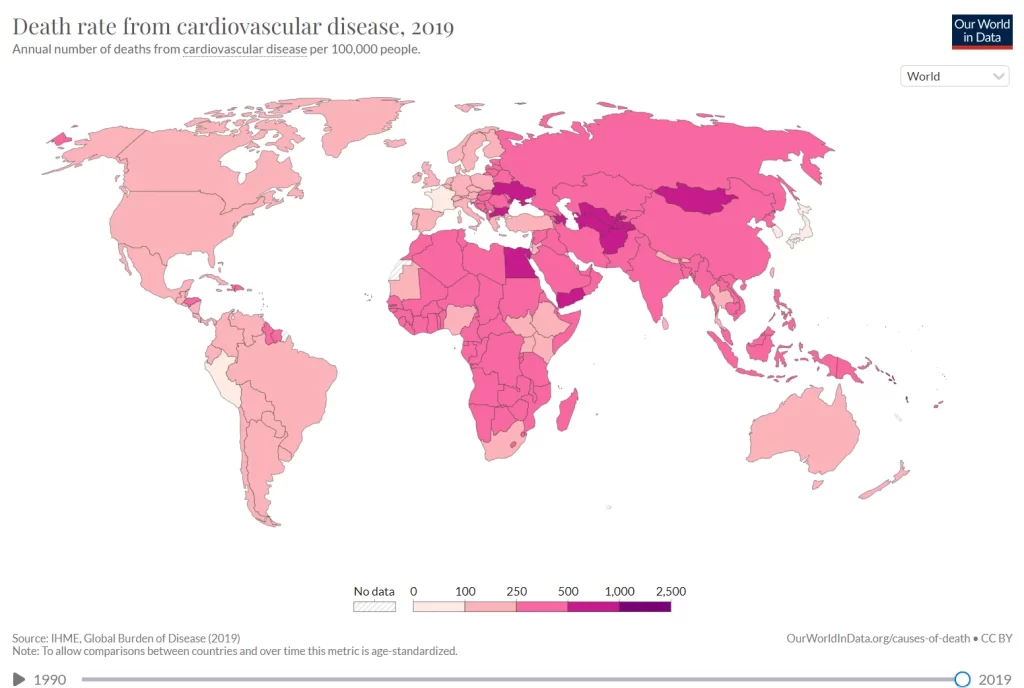
Source: IHME, Global Burden of Disease (2019)
The WHO agreed in 2013 on global mechanisms to reduce premature deaths from non-communicable diseases by 25% by 2025 through nine voluntary global targets. Two of these targets focus directly on management of CVDs by reducing the global prevalence of raised blood pressure by 25% as well as preventing heart attacks and strokes by providing at least 50% of eligible patients access to drug therapy and counselling. In addition, there is a target set for 80% availability of affordable basic technologies and medicines in both public and private healthcare facilities [6].
Key Takeaways
CVDs have become the leading cause of noncommunicable death globally in the 20th century. From the mid-1970’s a decline in mortality because of CVDs was reported in mostly high-income countries, with mortality levels typically falling by 40-80%. Studies have suggested that this could be due to several factors, including minimizing exposure to risk factors, improved medical management and screening as well as technology advances.
The disease burden of CVDs remains high and affects over 32% of the population. Low- and middle-income countries are most affected and out of 17 million premature deaths because of noncommunicable diseases, 38% are caused by CVDs. Populations in low- and middle-income countries who suffer from CVDs often do not have access to effective and equitable health care services which address their needs. As a result, detection is often late in the course of the disease and people demise at a younger age, often in their most productive years.
Patients with CVDs should have access to appropriate cardiovascular disease innovations (technology and medication) regardless of their socioeconomic status. Appropriate surgeries and medical devices which are lifesaving should be accessible and affordable for CVD patients.
References
[1] Alan D Lopez, Tim Adair, Is the long-term decline in cardiovascular-disease mortality in high-income countries over? Evidence from national vital statistics, International Journal of Epidemiology, Volume 48, Issue 6, December 2019, Pages 1815–1823, https://doi.org/10.1093/ije/dyz143
[2] Mensah GA, Wei GS, Sorlie PD, Fine LJ, Rosenberg Y, Kaufmann PG, Mussolino ME, Hsu LL, Addou E, Engelgau MM, Gordon D. Decline in Cardiovascular Mortality: Possible Causes and Implications. Circ Res. 2017 Jan 20;120(2):366-380. doi: 10.1161/CIRCRESAHA.116.309115. PMID: 28104770; PMCID: PMC5268076.
[3] Mehta NJ, Khan IA. Cardiology’s 10 greatest discoveries of the 20th century. Tex Heart Inst J. 2002;29(3):164-71. PMID: 12224718; PMCID: PMC124754.
[4] Oliver E, Mayor Jr F, D’Ocon P. Beta-blockers: Historical Perspective and Mechanisms of Action. Rev Esp Cardiol Engl Ed [Internet]. Available from: https://www.revespcardiol.org/en-beta-blockers-historical-perspective-mechanisms-action-articulo-S1885585719301100
[5] 10 heart drugs with weird origins [Internet]. [cited 2023 Feb 24]. Available from: https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/drug-cabinet/heart-drugs-with-weird-origins
[6] Cardiovascular diseases (CVDs) [Internet]. [cited 2023 Feb 24]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Table of Contents
