What is Budget Impact Analysis?
Pharmacoeconomic analyses in healthcare are paramount, because of the high costs of innovative technologies and limited possibilities of their funding. Budget Impact Analysis (BIA) is one such analysis that provides vital information for healthcare decision makers. [1]
Unlike economic evaluations, such as cost-effectiveness analysis (CEA), cost-utility analysis (CUA) and cost-benefit analysis (CBA) that evaluate the costs and consequences of healthcare; budget impact analysis (BIA) predicts the financial impact of the adoption and diffusion of innovation. Budget impact analysis (with budget impact models) also addresses the expected changes in expenditure of a healthcare system after adopting a new intervention. Decision-makers also use budget impact analysis for resource planning. [2-3]
Organisations who manage and plan healthcare budgets also use budget impact models to align pricing with resources, that is finding an optimal price for each intervention. This includes administrators of regional or national budgets, private health insurance plans, healthcare delivery organisations and employers who pay for healthcare. Each user’s requirement may differ, but each requires information on the financial impact of the adoption and diffusion of the new intervention. [2]
Though based on the principles of accounting, budget impact analysis is not an economic evaluation (includes cost-effectiveness analysis (CEA), cost-utility analysis (CUA) and cost-benefit analysis (CBA)). There are key distinct differences [Table 1] between the two [2][4]:
- Economic evaluations do not a model for the expected size of the patient population, however this is a requirement for budget impact analysis;
- Economic evaluations report health outcomes, whereas budget impact analysis report costs only;
- Economic evaluations present results as the discounted present value of costs in one period. Budget impact models report the costs for each year they occur with no discounting.
- Perform a budget Impact analysis and a cost-effective analysis (which determines whether an intervention provides value relative to an existing intervention), to support applications for reimbursement. Both analyses form part of a Health Technology Assessment (HTA).[4][5]
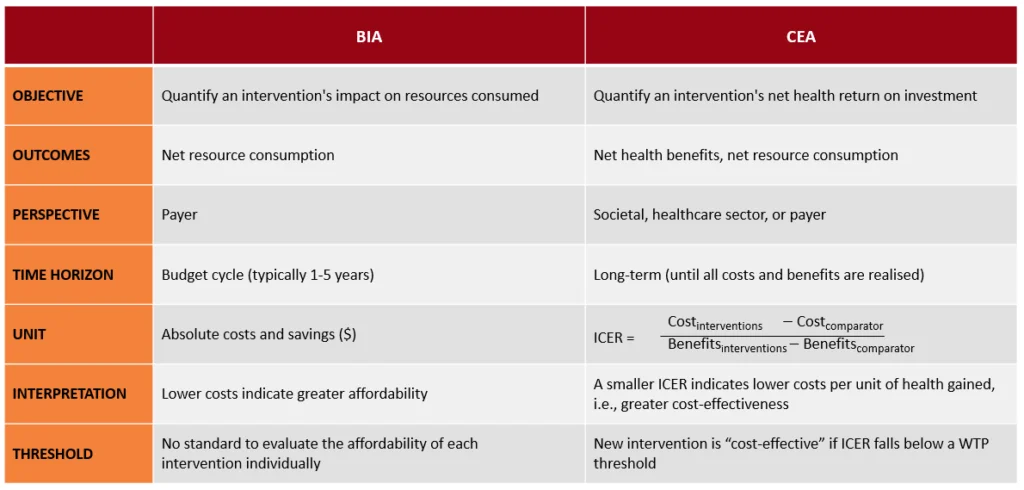
Table 1: Budget Impact Analysis compared with a Cost-Effective Analysis (Source:Carattini, 2011)
Budget Impact Modelling Framework
The proper design of an analytical framework [Figure 1] is a crucial step in budget impact analysis. It enables a practical comparison between the current treatment and condition, with the new scenario that would result from adopting a new intervention. The framework allows examination of the impact of the intervention on the healthcare system, by assessing disease, incidence, diagnosis and treatment, and resource and costs. The next step is to compare the total costs of each scenario to estimate the budget impact of the innovation. Researchers require certain inputs to construct the BIA modelling framework and enable data drive [2][3][6]:
- Size and characteristics of the affected population;
- The current intervention mix;
- The cost of the current intervention mix;
- The proposed intervention mix, including intervention under consideration;
- The cost of the new intervention mix;
- The cost of the new intervention mix, which includes the intervention under consideration;
- The use and cost of other health treatment-related healthcare services.
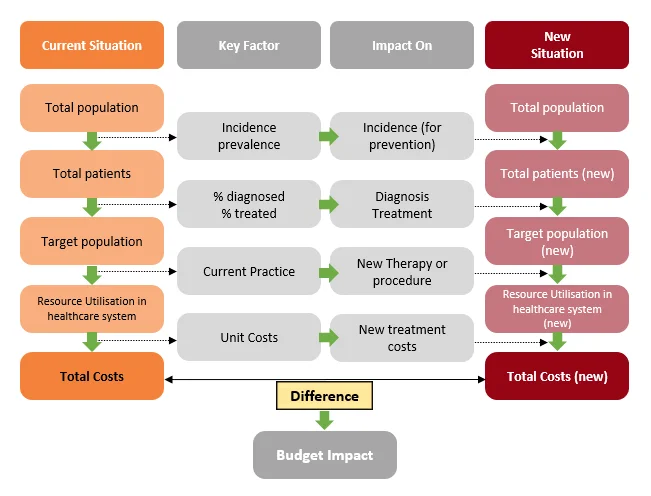
Figure 1: Budget Impact Analysis Model (Source: Leelahavarong, 2014, adapted from ‘Principles of good practice for budget impact analysis: report of the ISPOR Task Force on good research practices-budget impact analysis’, 2007).
Why is Budget Impact Analysis Important?
Budget impact analysis is an essential part of a Health Technology Assessment [3][7]. A budget impact analysis serves several important functions:
- To estimate financial consequences for a specialised population of implementing a new intervention or technology;
- A comprehensive analysis in a Health Technology Assessment, combined with a cost-effective analyses (CEA);
- To provide affordability data on innovations in healthcare at an optimal price for a specified population, prior to reimbursement;
- To serve as a budget and service planning tool that policy decision-makers can use to inform their allocation of resources after confirmed reimbursement of a technology;
- To provide a framework for stakeholders to examine different assumptions about the potential impact of new interventions on the technology mix, treatment costs, key success factors, and dynamic pricing; and
- To predict how a change in the mix of interventions used for a condition affects the trajectory of spend on that condition.
In a cost-conscious market, providers are under extreme pressure to show the real value of their products. Budget impact analysis is as important as a cost-effective analysis to build a firm position for adopting a new intervention. It is flexible enough to allow efficient estimates of the cost of treatment for a certain condition and display how each new intervention impacts on total treatment. [3][7]
Benefits of Budget Impact Analysis
Budget impact analysis complements the information for a comprehensive Health Technology Assessment. It is complementary to more established types of economic evaluations, namely cost-effectiveness analysis, by providing additional information on the financial consequences of reimbursement of new technologies.[1] However, as a comprehensive HTA takes time and is labour intensive, decision-makers may use a budget impact analysis in isolation to determine the financial impact of an innovation.[4]
Budget impact analysis also assesses affordability by estimating an intervention’s short-term net costs from the payer’s perspective.[2][8] The outcomes of a budget impact analysis reflects scenarios with a specific set of assumptions and data inputs of interest to the decision makers. [1][8] It provides a structured framework that allows users to see how different assumptions results in changes in the treatment mix and cost of treating that condition. [9]
Although a new intervention is generally expensive, it may reduce overall costs because of reduced hospital days and out-patient visits. A budget impact analysis that shows a reduction in overall disease cost, is an added motivation for reimbursement. [8]
Practical steps in Getting Started with a Budget Impact Analysis
Researchers apply six steps to conduct a budget impact analysis. These are preceded by developing an analytic framework to guide data collection and populate a budget impact model with data relevant to the budget holder [3] [8] [9] [10]:
Characterise the population
A focused description of the target population improves the relevance and accuracy of budget impact results. The population is identified by using a funnel-down approach. Firstly, identify patients who qualify medically and in accordance with the guidelines (but may not necessarily choose to be treated with the new technology). Then narrow down the population using epidemiology data to arrive at the number of eligible patients. Sometimes, this population may be further restricted on the basis of HTA decisions; it is important to consider subgroups within the disease area.
Once the population is estimated, they are separated into Incident and Prevalent cohorts. The prevalent population is the population of patients who are eligible for the new technology today, while the incident population are those patients who are newly diagnosed and will be eligible for the technology once it comes onto the market. Separating the population into these groups enables budget holders to account for cohorts of patients with varying years of treatment.
Select the Time Horizon
Decision makers often prefer shorter horizons. Allow for flexibility so that decision maker can choose any period from 1 to 5 years. Longer horizons are useful only when the population and treatments are likely to remain stable. Markets are ever-changing and predicting the impact of potential comparator treatments may influence the prediction of a realistic budget impact analyses, should the time horizon be too long.
Current and Future Treatment Mix
Clarity on the positioning (new or substitute) of the new intervention will influence how the market shifts. In budget impact analyses, decision makers are interested in comparing budgets with, and without the new technology. Firstly, obtain or estimate the mix of treatments currently used within the health plan, so changes in the treatment mix over the remaining budget time horizons can be projected on the basis of historical trends, as seen in the claims data. To further develop the new technology’s budget, the uptake of the technology, as well as the change in the mix of treatments and their market shares over the analysis time horizon, will need to be determined.
Other factors to be considered are to whether the new technology will be a substitute for another technology, or will it augment the current technologies in some manner? These factors influence the projected change in market share mixes for treatments within the budget scenarios over time.
Estimate Intervention Costs
Adherence to interventions impact on cost and outcomes and consider discounting if the time horizon is long. The primary cost component of the new technology is the acquisition cost, which can be estimated from published list prices, until true negotiated prices are established. Other costs, such as administration and monitoring need to be factored in, especially if the new technology is competing with other treatments that do not require these additional costs.
In addition, the cost of treating adverse events should be considered; it may be advantageous to include this cost within the budget impact analyses for credibility purposes. As budget impact analyses are created to represent real-world budgets, the inclusion of rebates and discounts need to be considered too. Brand versus generic versions of treatments, as well as treatment adherence may also have a significant impact on the cost of a new technology.
Estimate Changes in Disease-Related Costs
Data from clinical trials should be considered for acute diseases, while progression models and effectiveness estimates are used for chronic diseases. Disease costs for acute diseases, are usually straightforward. Resource use and costs could be micro-costed or estimated on a per-event basis from publications and/or analyses of claims data.
For chronic diseases, these costs are often more complicated to estimate, and different levels of disease severity would need to be considered. Estimated costs may be readily available from healthcare claims, registries and or other longitudinal data in which patients are followed. If the changes in disease related costs are expected to occur outside of the budget impact model time horizon, then they will not change the model’s budget estimates. However, these costs can be presented alongside the budget-impact estimates as clinical benefits to help the budget holder understand the value of the additional budget needed for the curative treatment.
Present Budget Impact and Health Outcomes
Results are presented as costs per treated person per month and are presented alongside health outcomes studies. Generally, budget impact analyses are presented in tabular and graphic formats, on an annual basis and disaggregated at a level that makes sense for the budget holder. For example, costs may be presented at pharmacy level versus the medical budget level. Costs are also undiscounted as actual costs are important. Presenting budget impact analyses alongside health outcomes studies to the budget holder also inform them of the benefits(s) received for the potential increase in costs.
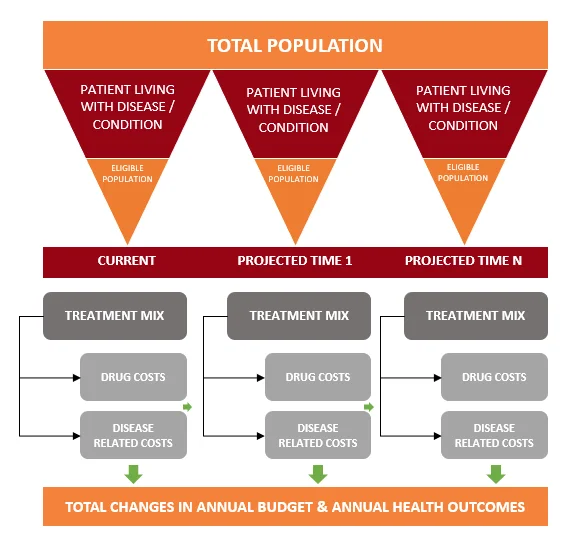
Figure 2: Six Steps for Estimating the Budget Impact (Source: Steuden 2017).
Budget Impact and Cost-Effectiveness Calculations
New healthcare technologies generally enter the marketplace at a higher cost than current approved comparator technologies, lending thinking to the possibility that they are more expensive and not affordable. However, the new technology may have improved clinical efficacy and/safety, so costs of the new technology could be offset (partially or fully) by decreased costs associated with treating patients with other medical resources. Table 2 below, illustrates the calculation of a budget impact compared with a cost-effectiveness analysis on a 1-year time horizon.
Scenario: A new biologic (Syenivolab) is approved to treat patients with moderate to severe Rheumatoid Arthritis in adults over 18 years. Syenivolab is administered monthly, to keep patients in remission. As it is a biologic, Syenivolab is more expensive than other treatments on the market, but its increased efficacy reduces flairs and prevents additional treatments. The current approved medication is also given once a month.
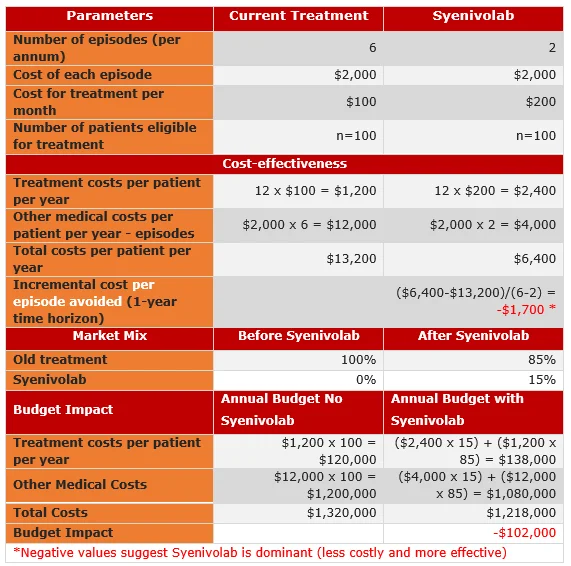
Table 2: Calculation of the Budget Impact with Cost-effectiveness of Syenivolab (Adapted from Rascati: 2021).
Static vs. Dynamic Approaches to Budget Impact Analysis
When calculating budget impact, it is important to account for the size of the total population and/or the size of various subgroups. There are two different approaches: a static or a dynamic approach. A static approach is used when the size of the total population and the subgroups (if they exist) presumes to remain constant. A dynamic approach is used when the introduction of the new technology could cause the size of the total population and/or subgroups to change over time and across budgets. The size of the population may change, when the new technology; decreases mortality or disease progression; changes the duration of treatment or decreases disease related complications.[10]
- Static Approach: With this approach, the size of the eligible population is assumed to remain constant across the annual budgets. When the new technology is launched, the calculation of the costs and outcomes within the budgets become a simple cost calculation or the expected value calculation. Thus, costs and outcomes incurred by patients within the population are weighed by the proportion of patients within the population receiving the technologies considered in the analysis.
- Dynamic Approach: As the new technology changes the size of the population over time, the dynamic approach is an exercise in managing cohorts to accurately provide for the proper number of individuals in each of the budget scenarios. With this approach, it is important to differentiate the incident from the prevalent population. Start with the prevalent cohort of patients in the 1st year [Figure 3], adding in the small number of recently diagnosed (incident) patients in the same year (Prevalent cohort + Incident cohort 1). These patients will receive the new technology. In the 2nd year, another set of patients will receive the diagnosis and be eligible for the new technology (Incident cohort 2). In the 3rd year, another new set of patients will be eligible for the new technology on diagnosis (Incident cohort 3). Thus, every year a new cohort enters the system. At the same time, each year patients are exiting the system (cured, in remission or death). From these population counts, within each budget year, the budgets are estimated with these scenarios containing a varying number of patients treated with the technology for the different years. These calculations can be more complex; therefore, health economists tend to use Markov models for these situations.
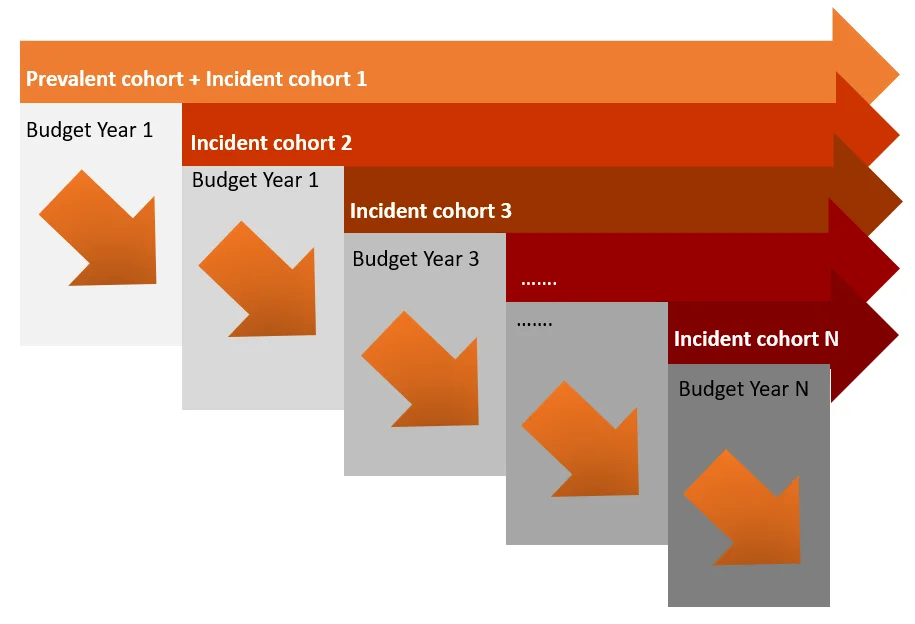
Figure 3: Managing Cohorts in a Dynamic Budget Impact Analyses (Source: Rascati: 2021)
Summary
A budget impact analysis is used to assess whether adopting a new health innovation is affordable, given resource and budget constraints [3]. Budget impact analysis is important as part of a Health Technology Assessment when combined with a cost-effectiveness analysis for reimbursement. It is also important for budget and forecast planning, estimating the impact of health technology changes on health insurance premiums and estimating potential fiscal impact on pursuing an intervention at national level [3] [7].
Budget impact analysis may be conducted in isolation or part of a comprehensive analysis with complementary economic evaluations for HTA [1] [4]. In addition, managers can make strategic decisions, as BIA estimates the financial feasibility of a new intervention in a healthcare [6]. The budget impact analysis services at Syenza determine the optimal price of innovations by identifying opportunities for dynamic pricing and outcomes-based pricing. Our budget impact models also align pricing with value, and articulate key success factors in value-based pricing frameworks. Learn more here and contact us for further details.
References
[1] R. I. Yagudina, A. U. Kulikov, V. G. Serpik and et.al, “Concept of Combining Cost-Effectiveness Analysis and Budget,” Value in Health Regional Issues, vol. 13C, pp. 61-66, 2017. Link.
[2] S. D. Sullivan, J. A. Mauskopf, F. Augustovski and et.al, “Budget Impact Analysis—Principles of Good Practice: Report of the ISPOR Task Group,” Value in Health, vol. 17, pp. 5-14, 2014. Link.
[3] P. Leelahavarong, “Budget Impact Analysis,” J Med Assoc Thai, vol. 97, no. Suppl 5, pp. S65-S71, 2014.
[4] Health Information and Quality Authority, “Guidelines for the Budget Impact Analysis of Health Technologies in Ireland,” Health Information and Quality Authority (HIQA), Dublin, 2018.
[5] L. Garattini and K. van de Vooren, “Budget impact analysis in economic evaluation: a proposal for a clearer definition,” The European Journal of Health Economics, pp. 449-502, 2011.
[6] M. T. Silva, E. N. da Silva and M. G. Pereira, “Budget impact analysis,” Epidemiol. Serv. Saude, vol. 26, no. 2, pp. 1-4, 2017.
[7] J. B. Babigumira, “Budget Impact Analysis,” School of Public Health University of Washington, Seattle, 2017.
[8] A. Bilinski, P. Neumann, J. Cogen and et.al, “When cost-effective interventions are unaffordable: Integrating cost-effectiveness and budget impact in priority setting for global health programs,” Plos Medicine, vol. 14, no. 10, pp. 1-10, 2017.
[9] L. Steuten, “Budget Impact Analysis,” University of Washington, Seattle, 2017.
[10] Rascati K. Chapter 12: Budget-Impact Analysis. In: Essentials of Pharmacoeconomics. 3rd edition. LWW; 2021.
Table of Contents
