Cardiovascular diseases (CVDs) remain the leading cause of death worldwide, claiming millions of lives annually and presenting significant challenges to healthcare systems and economies (1,2). With CVD innovations driving progress, the prevalence of CVDs is increasing due to factors such as aging populations, urbanisation, and lifestyle changes, creating an urgent need for advanced prevention and management strategies.
The World Health Organization (WHO) reports that CVDs account for approximately 32% of all global deaths, with a significant portion occurring in low- and middle-income countries (LMICs) and of these deaths, 85% were due to heart attack and stroke. (2,3). The economic implications are equally staggering, with healthcare systems burdened by the direct costs of treatment and the indirect costs of lost productivity due to illness and premature death. In the United States, the financial impact of CVDs reached $417.9 billion between 2020 and 2021 alone (2,4). This emphasises the urgent need for innovative solutions that can effectively address this global health crisis.
In response to these challenges, the medical community is increasingly focusing on cutting-edge technologies and evidence-based interventions to curb the CVD epidemic. This article explores the latest advancements in cardiovascular disease prevention, diagnosis, and treatment. It offers insights into how these CVD innovations are transforming patient outcomes and shaping future healthcare strategies. By examining the interplay of technological advancements, public health initiatives, and policy frameworks, we aim to provide an overview of the current landscape and future directions in cardiovascular health.
Understanding the Global Burden of Cardiovascular Diseases
Prevalence and Incidence
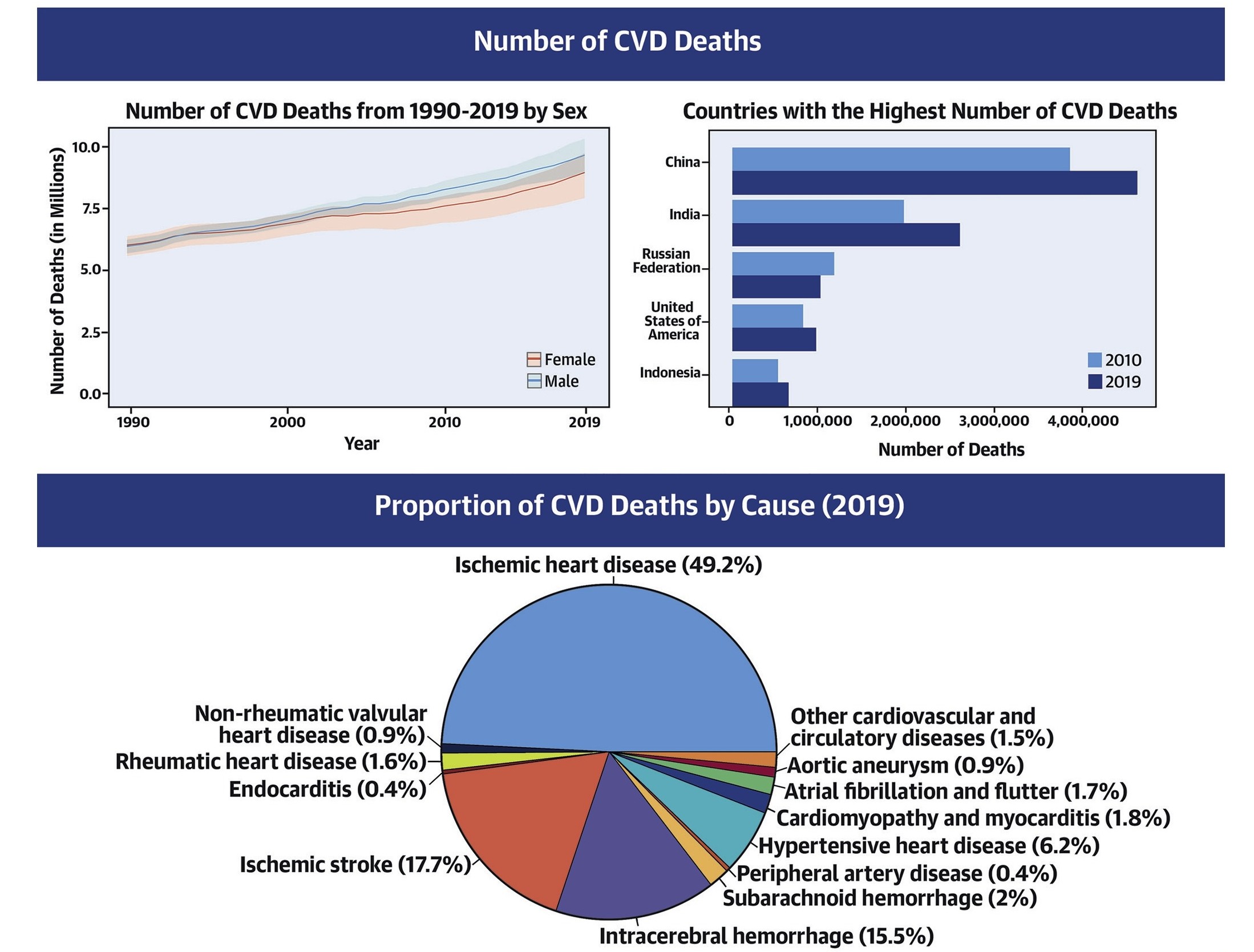
CVDs remain a critical public health issue worldwide, characterised by significant prevalence and incidence rates that vary across regions and populations. Global data highlights the substantial burden of CVDs, with ischemic heart disease and stroke being the most prevalent forms (4). According to the World Health Organization, CVDs account for 32% of all global deaths, with an estimated 17.9 million people dying from CVDs in 2019 (3). Of these deaths, 85% were due to heart attack and stroke, emphasising their impact on health systems and communities. Over three-quarters of CVD deaths occur in LMICs. (1,5) Furthermore, 38% of the 17 million premature deaths from noncommunicable diseases in 2019 were caused by CVDs (3). These statistics highlight the pressing need for comprehensive prevention and intervention strategies.
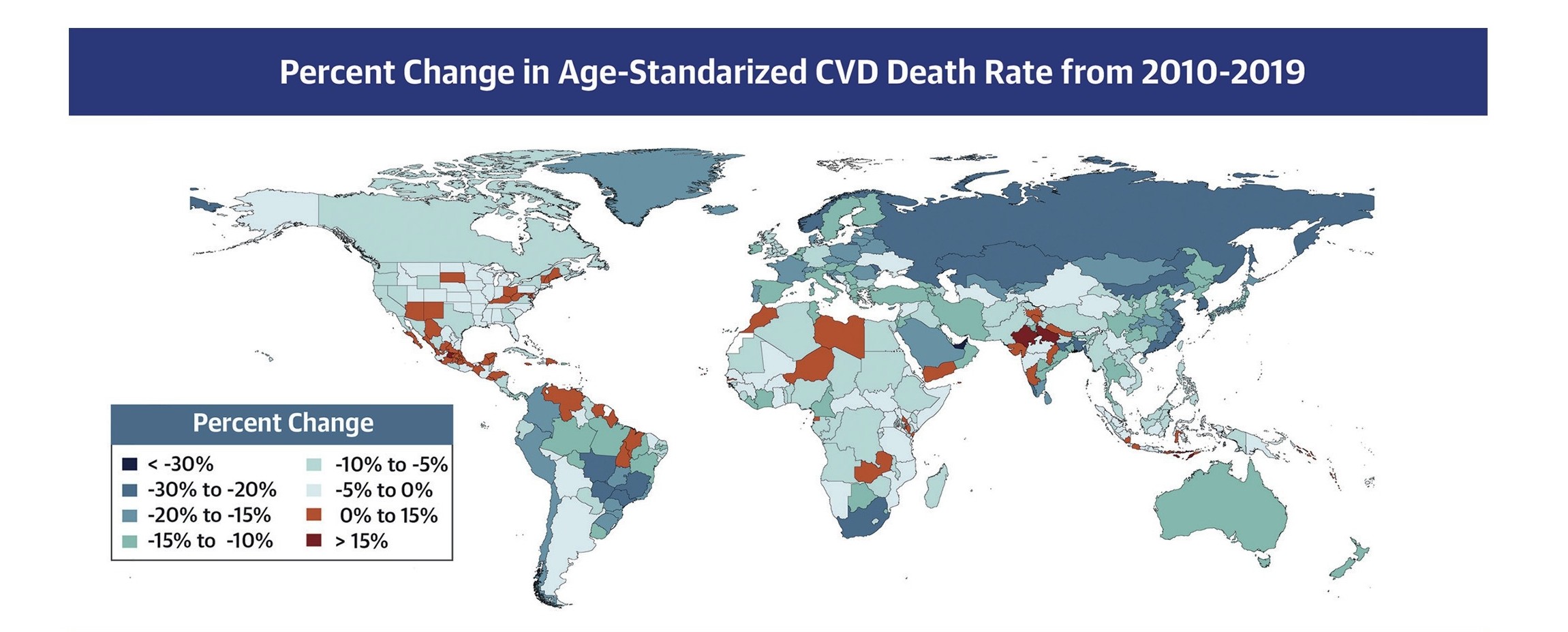
Regional Variations and Risk Factors
In the United States, CVDs were responsible for 941,652 deaths in 2022, with coronary heart disease (CHD) and stroke accounting for 39.5% and 17.6% of these fatalities, respectively (4). Hypertension, a significant risk factor, affects 46.7% of U.S. adults, while diabetes was diagnosed in 10.6% of adults, with additional undiagnosed and prediabetic cases contributing to the burden (4). In sub-Saharan Africa, CVD prevalence and incidence have risen due to demographic transitions (6–8). Non-communicable diseases (NCDs), including CVDs, increased from 18.6% of DALYs in 1990 to 29.8% in 2019. CVDs accounting for 13% of all-cause mortality and 37% of NCD-related deaths (7,9). Hypertension, affecting nearly half the population over 25, is a major factor, yet awareness and treatment remain low (6).
Projections indicate a decline in age-standardized DALY rates per 100,000 population across all modifiable CVD risk factors from 2025 to 2100 (1). However, high systolic blood pressure (SBP) and high body-mass index (BMI) are expected to remain prevalent, particularly in South Asia and Southeast Asia, East Asia, and Oceania (1). The burden of modifiable CVD risk factors is anticipated to shift from high-middle to low-middle socio-demographic index (SDI) regions by 2100, highlighting the need for targeted interventions (1).
Overall, the increasing prevalence and incidence of CVDs globally, particularly in LMICs and SSA, emphasise the urgent need for effective prevention and intervention strategies tailored to regional and demographic health challenges. Addressing these disparities through comprehensive healthcare access and targeted lifestyle interventions is crucial for mitigating the global impact of cardiovascular diseases.
Innovations in Prevention, Diagnosis, and Treatment
Prevention Strategies
Preventive strategies are evolving to incorporate technological innovations and community-based approaches. Mobile health applications, such as the Stroke Riskometer, empower individuals to assess their risk and adopt healthier lifestyles by providing personalised feedback and recommendations (2). Public health campaigns emphasise the importance of the American Heart Association’s ‘Life’s Essential 8’. It includes recommendations for maintaining optimal cardiovascular health through regular physical activity, healthy eating, and smoking cessation (4).
Community health initiatives are also playing a crucial role in prevention. For example, workplace wellness programs encourage employees to engage in regular physical activity and maintain a balanced diet, reducing the risk of CVDs (6,9). Educational programs in schools and communities aim to raise awareness about the importance of cardiovascular health and promote healthy lifestyle choices from a young age (1).
Diagnostic and Treatment Innovations
Advancements in diagnostic technologies are transforming the early detection and management of CVDs. Artificial intelligence (AI) and machine learning models, such as HTN-AI, are being developed to analyse vast datasets from electronic health records and ECGs, enabling more accurate risk prediction and personalised treatment plans (12,13). These technologies allow for the identification of subtle patterns and risk factors that may be overlooked by traditional diagnostic methods, facilitating earlier interventions and better patient outcomes (2).
In terms of treatment, polypills, which combine multiple medications, have been shown to improve adherence and reduce cardiovascular events in at-risk populations (2). By simplifying medication regimens, polypills enhance patient compliance and reduce the likelihood of adverse events associated with multiple drug interactions (2). Regenerative medicine approaches, such as iPSC-derived cardiomyocyte allografts, hold promise for treating heart failure by repairing damaged heart tissue and improving cardiac function (14,15). These iPSC-derived therapies not only offer the potential for personalised heart repair but also reduce the risk of immune rejection, as they can be tailored to match the patient’s genetic profile, paving the way for more effective and individualised treatment strategies (14,15).
Barriers to Progress and Global Efforts
Barriers to Progress
Despite these advancements, significant barriers remain in addressing the CVD epidemic. Socioeconomic disparities, cultural beliefs, and healthcare access issues hinder the implementation of effective prevention and treatment strategies, particularly in LMICs (7). In many African countries, traditional beliefs and practices can impede the adoption of modern healthcare interventions, necessitating culturally sensitive approaches to health promotion (6). The lack of infrastructure and trained healthcare professionals poses challenges to delivering comprehensive cardiovascular care (1).
Global Efforts and Strategic Goals
Global health organisations and governments are working collaboratively to address these challenges through strategic initiatives and policy reforms. The WHO’s Sustainable Development Goal 3.4 aims to reduce premature mortality from non-communicable diseases by one-third by 2030, emphasising the need for integrated health systems and community engagement (2). In Africa, the Pan-African Society of Cardiology is leading efforts to improve hypertension control through task-sharing with community health workers and enhancing access to essential medications (6). These efforts highlight the importance of global cooperation and targeted interventions in reducing the CVD burden.
Conclusion
Addressing the global burden of cardiovascular diseases requires a multifaceted approach. It requires leveraging technological innovations, public health strategies, and policy reforms (7). By prioritising prevention, enhancing healthcare access, and fostering international collaboration, we can improve public health outcomes and reduce the impact of CVDs (1,2). As we continue to advance in medical research and healthcare delivery with CVD innovations, a collective commitment to these goals will pave the way for a healthier future, with reduced mortality and improved quality of life for affected populations (16).
References & Citations
- Chong B, Jayabaskaran J, Kueh M, Goh R, Li H, Foo R, et al. The projected global burden of modifiable risk factors on cardiovascular disease from 2025 to 2100. European Heart Journal. 2024 Oct 28;45(Supplement_1):ehae666.2617.
- Feigin VL, Brainin M, Norrving B, Martins SO, Pandian J, Lindsay P, et al. World Stroke Organization: Global Stroke Fact Sheet 2025. International Journal of Stroke. 2025 Feb;20(2):132–44.
- Cardiovascular diseases (CVDs) [Internet]. [cited 2025 Mar 10]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- 2025-Statistics-At-A-Glance.
- 2025-statistics-at-a-glance.pdf [Internet]. [cited 2025 Mar 10]. Available from: https://www.heart.org/en/-/media/phd-files-2/science-news/2/2025-heart-and-stroke-stat-update/2025-statistics-at-a-glance.pdf
- Mtintsilana A, Mapanga W, Craig A, Dlamini SN, Norris SA. Self-reported hypertension prevalence, risk factors, and knowledge among South Africans aged 24 to 40 years old. J Hum Hypertens [Internet]. 2025 Feb 24 [cited 2025 Mar 9]; Available from: https://www.nature.com/articles/s41371-024-00957-8
- Oguta JO, Breeze P, Wambiya E, Kibe P, Akoth C, Otieno P, et al. Application of decision analytic modelling to cardiovascular disease prevention in Sub-Saharan Africa: a systematic review. Commun Med. 2025 Feb 22;5(1):46.
- Lubbe C. Hypertension in Young South African Adults [Internet]. Syenza News. 2025 [cited 2025 Mar 10]. Available from: https://news.syenza.com/hypertension-young-adults-prevalence-knowledge-south-africa/
- Carapinha JL. CVD Prevention Models in Sub-Saharan Africa: Insights and Gaps [Internet]. Syenza News. 2025 [cited 2025 Mar 10]. Available from: https://news.syenza.com/cvd-prevention-models-sub-saharan-africa-insights-gaps/
- Roth S, Fernando C, Azeem S, Moe GW. Is There a Role for Ivabradine in the Contemporary Management of Patients with Chronic Heart Failure in Academic and Community Heart Failure Clinics in Canada? Adv Ther. 2017 Jun;34(6):1340–8.
- Watson B. The Only Checklist You Need For Lifelong Good Health [Internet]. Xcode Life. 2023 [cited 2025 Mar 10]. Available from: https://www.xcode.life/genes-and-health/good-health-checklist/
- Al-Alusi MA, Friedman SF, Kany S, Rämö JT, Pipilas D, Singh P, et al. A deep learning digital biomarker to detect hypertension and stratify cardiovascular risk from the electrocardiogram. npj Digit Med. 2025 Feb 22;8(1):120.
- Carapinha JL. Hypertension Detection: HTN-AI Model for Cardiovascular Risk Stratification [Internet]. Syenza News. 2025 [cited 2025 Mar 10]. Available from: https://news.syenza.com/hypertension-detection-model-htn-ai-cvd-stratification/
- Jebran AF, Seidler T, Tiburcy M, Daskalaki M, Kutschka I, Fujita B, et al. Engineered heart muscle allografts for heart repair in primates and humans. Nature [Internet]. 2025 Jan 29 [cited 2025 Mar 9]; Available from: https://www.nature.com/articles/s41586-024-08463-0
- Carapinha JL. Engineered Heart Muscle Allografts Show Promise in Heart Repair [Internet]. Syenza News. 2025 [cited 2025 Mar 10]. Available from: https://news.syenza.com/engineered-heart-muscle-allografts-promise-heart-repair/
- Chan J, Narayan P, Fudulu DP, Dong T, Vohra HA, Angelini GD. Long-term clinical outcomes in patients between the age of 50–70 years receiving biological versus mechanical aortic valve prostheses. European Journal of Cardio-Thoracic Surgery. 2025 Feb 4;67(2):ezaf033.
Table of Contents

